Virginie Papadopoulou, PhD
Bubbles in Blood ꟷ from Sea and Space, to Health Applications

This text is reproduced from the newsletter article I contributed to the UK Space Environments Association newsletter (April 2017):
More technical details about some of the topics discussed here can be found in the 2014 open access article “Circulatory Bubble Dynamics: From Physical to Biological Aspects”, by Papadopoulou V, Tang M-X, Balestra C, Eckersley RJ, Karapantsios TD, published in Advances in Colloid and Interface Science.
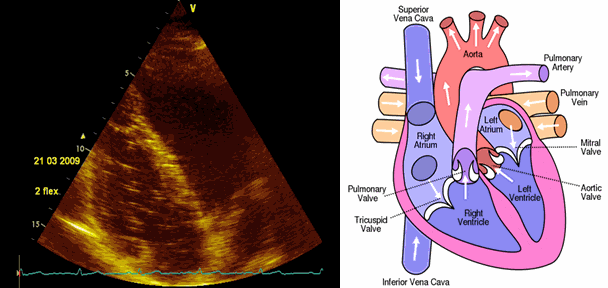
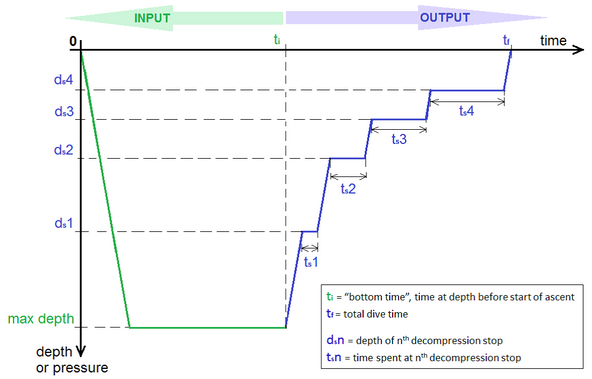
Gas bubbles in blood can cause embolization with potential serious consequences. In the case of decompression-induced bubbles from scuba diving or extravehicular space walks, this can result in decompression sickness (DCS). DCS symptoms range from skin manifestations to coma or death, often presenting with severe joint pain which earned its nickname of ‘the bends’. Divers inhale their breathing gas supply at ambient pressure throughout the dive. During ascent (decompression), the tissues start releasing excess dissolved gas, creating bubbles that go to the blood stream, possibly through the lymphatic pathway. Most dives, even conservative, no-decompression, shallow dives, create some degree of bubbles visible using ultrasound imaging post-dive. Bubbles can cause problems by direct mechanical effects in tissues or in the circulation (blockages, shear stress etc) or through the body’s associated inflammatory responses to them. Circulating bubbles in venous blood are normally filtered by the lungs which trap emboli larger than 8μm. However, when these bubbles are too large or too many and overload the pulmonary filter, or paradoxically enter the arterial circulation through arteriovenous shunts, they effectively become arterial gas emboli flowing in increasingly smaller vessels towards the brain potentially causing neurological DCS.
Scuba diving remains a relatively safe activity with respect to DCS incidence, however probabilistic decompression models based on big databases for estimating the risk of a particular exposure do not relate to physiological mechanisms. Inter- and intra- personal differences in risk, even for a same diving profile, are well-documented and these physiological variables are not accounted for in current algorithm implementations. A new endpoint, beyond simply DCS/no DCS, is needed for validating decompression models and algorithms is needed. This would allow researchers to assess preconditioning interventions (specific exercise, hydration, supplements pre-dive to lower decompression stress) and inter-personal physiological differences in risk.
Scuba diving incorporates stressors such as pressure, immersion, temperature and exercise, causing physiological adaptations on different timescales, as both short and long-term coping mechanisms are triggered during and after the dive. Having a comprehensive assessment of this stress in healthy diving could prevent long term effects, and investigate effective strategies for short term effects reversal, with applications to oxidative stress and gas emboli responses in biomedical fields. The aim is to develop new techniques towards the quantification of hyperbaric decompression stress, as an environmental cardiovascular personalized stress index. Understanding the complex formation, growth and rheological behavior of bubbles as they flow in blood is important for safe sea and space exploration, but also links to other fields in health applications.
Interestingly, there is an application where microbubbles are injected in the blood on purpose – microbubble contrast agents for ultrasound imaging. These are very different to the decompression bubbles produced in diving or gas emboli that can cause problems during surgical procedures. Ultrasound imaging is a non-ionizing, real-time, portable and relatively cheap imaging technology. Nevertheless blood appears dark on standard Bmode ultrasound due to the poor scattering of sound from red blood cells. Microbubbles, lipid-stabilized gas bubbles of about 2μm in size, oscillate with the transmitted ultrasound wave compression and refraction due to their compressible gas core. These oscillations can be further amplified by matching the transmitted ultrasound pressure to the natural resonance from the diameter bubbles. As such, the signal from microbubbles is extremely strong and they act as a blood pool marker or contrast agent. They can be administered as a single bolus or slow infusion, resulting in an imaging window around 5min to 30min respectively.
Ultrasound contrast microbubbles are clinically approved for a number of diagnostic applications in Europe and the USA, in particular assessing perfusion defects in the heart. Their unique oscillatory behavior under ultrasound, as their compression and expansion phases are not completely antisymmetric, has been used to develop specific imaging modes to selectively display only blood signal. These agents are also being investigated for therapy applications, for instance by enhancing vascular permeability of chemotherapy drugs locally for cancer. Recent advances in ultrasound hardware in the last few years also allow for the first time frames rates as high as 20,000 frames per second. New super-resolution techniques breaking the fundamental resolution of ultrasound have been demonstrated in vivo with the ability to image vessels as small as a few microns in depth with no penetration depth limit.
* * *
These state of the art ultrasound techniques can also be applied to health monitoring and physiological research. Ultrasound is particularly well-suited to repetitive and portable experimentation on healthy individuals (as opposed to ionizing modalities such as X-ray, CT or PET and costly bulky MRI rooms). Biomedical engineering lies at the cross-roads between physics, mathematical modelling, computer science and biological or medical questions. Advanced techniques from multiscale modelling, time series analysis, systems medicine or cutting-edge signal processing and imaging techniques can be tailored to particular medical applications.
From the pioneering dives of Jacques Cousteau, we have been fascinated by exploration and recreational diving is today a tremendously popular activity. Research in, and for, the most extreme, fascinating environments at the limit of human exploration presents the ideal platform to engage children in science. Diving for recreation presents new challenges, as the acceptable level of risk is inherently different to commercial or military diving. The good track record of occupational health with regards to occupational decompression nowadays is a testament to the progress made since the first bridge and tunneling construction projects where many workers died or became paralyzed.
Nevertheless, I do not think DCS risk should be the only reason to study decompression physiology. In professional diving, we could envisage taking this knowledge forward to improve the safety and ability of workers to function at depth and recover quickly, whilst minimize the adverse long term effects of these extreme exposures. Importantly in the recreational setting, we have in a matter of decades, gone from fit, male, young divers to a general population diving as they get older, with pre-existing medical conditions. Most of the available testing of specific decompression procedures has been done in very controlled cases (square profiles) and for a typical military diver. It is increasingly obvious that this cannot be directly extrapolated to this new population doing multiday, multilevel diving. The recreational population is also increasingly pushing physical and mental limits of their sport, demonstrating record-breaking technical multi-gas decompression diving in deep, cold and overhead environments.
This new type of diving has opened an opportunity to redefine what we mean by environmental physiology research. Moving away from a targeted sample of individuals, we are now being truly inclusive and investigating personal responses to external stressors. Similarly, as commercial space exploration gains public attention, I would expect the study of space physiology to shift from astronauts, extremely selected individuals, to a general population eager to experience “Space”. The opportunity lies in developing new procedures for targeting our current understanding to each individual. Ultimately, the clinical picture is determined by both short and long space- and time-scales involved in stressor events and our ability to study the complex feedback loop of homeostasis imbalance and attempt at re-regulating accordingly.
Paradoxically, despite its apparent specialized focus, I would argue that research in extreme and environmental physiology has always been inclusive. Inclusive because we study the “outlier” athlete that lies many standard deviations away from how other people respond to a particular stressor. Inclusive because we study adaptations to the extreme environment that most people go to great lengths to avoid. Increasingly, however, it is inclusive because we want to personalize our understanding to individual physiology. I strongly believe that this understanding can have applications to medical health, just as new technologies allow advances in environmental physiology.
For such translations we need cross-disciplinary, international collaborative networks. We also need support from research funding agencies to facilitate higher-risk creative, disruptive innovations and encourage collaboration between hyper-specialized fields. Accounting for physiological variability, as well as developing and validating new multidisciplinary tools and models for personalizing prevention procedures and treatment outcomes, is key for safe Sea and Space exploration. It is also key for Health.
COPYRIGHT © ONEWEB 2012 | ALL RIGHTS RESERVED
PRIVACY STATEMENT | TERMS & CONDITIONS